Site selection, site rotation and tips for injecting insulin
Education is everything
There are a variety of ways insulin can be delivered, either through syringes, plastic prefilled insulin pens, refillable insulin pens or an insulin pump. Each of these devices delivers insulin through the needle into the fatty layer just beneath the skin’s surface. Insulin works best when it is injected into this layer as it gives a more even absorption of insulin into the blood stream.
If insulin is injected into the muscle layer, your body may absorb it too quickly, which can lead to low blood glucose levels. It also might not last as long in the body as it should.
Using needles that are the right length (usually 4-6mm) can help you avoid injecting into the muscle layer. These needles also tend to be thinner and are therefore less likely to cause pain when injecting. Some people may need to use longer needles, so it is always best to check with your healthcare team about the size of needle that is right for you.
Using a new needle each time you inject is also recommended, as needles can become damaged with repeated use. This can’t be seen with the naked eye but is noticeable when looking at a needle under a microscope. Reusing needles can damage the skin and increases the risk of pain and bleeding at the injection site. Needles and syringes are available free for people with diabetes who use insulin injections.
Choosing where to inject is another important consideration. Typically places where you can inject insulin include:
|
 |
When injecting insulin into the abdomen (tummy) avoid areas close the belly button and groin area. As a guide, think about the size of a twenty-cent piece or a two-finger width, and avoid injecting within that space around the belly button.
Insulin needs to be injected into fat, so it is important that each site has enough of a fat layer and is somewhere you can reach comfortably. The outer area of the upper arm or the buttock area can be more difficult to reach and therefore may not be a good option for everyone.
You should also avoid areas close to scars, moles, or skin blemishes as these can interfere with the way your body absorbs insulin. Stay clear of broken blood vessels and varicose veins as well. Your diabetes healthcare team can help work out which injection sites are best for you.
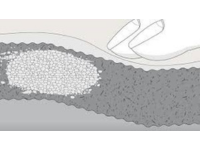
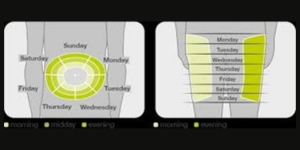
Changing insulin injection/pump sites is also an extremely important part of diabetes care. This is called site rotation and means following a regular pattern as you move the injection or pump site location around your body. Moving the place where you inject each time helps to avoid the build-up of fatty tissue called lipohypertrophy. This build-up of fatty tissue usually appears as a raised fatty lump under the skin. However, it is not always visible. It is therefore a good idea to routinely feel the areas used for injections by running your fingers over the area, feeling for any fatty lumps. These lumps can sometimes become painful and can change the way insulin is absorbed, leading to increased insulin doses and unpredictable glucose levels.
In time these fatty lumps can disappear once they are no longer being used for injections. These areas should only be used again once they have fully healed. Your health care team will regularly monitor your injection sites as part of your ongoing care. When you next visit your doctor or diabetes educator ask them to check your injection sites and have them checked at least every year.
Sometimes changes in your daily routine may require a change in your rotation pattern. Avoid injecting into an area that you will use during exercise if you are planning on exercising right after your injection. For example, if you inject into the leg and are planning on going for a walk or run, consider using an alternative site as exercise causes insulin to be absorbed more quickly and can lead to low blood sugar.
Other considerations when injecting insulin include:
- Using insulin at room temperature - this can reduce pain when injecting.
- Don’t use insulin that is discoloured.
- Always check the insulin use by date.
- Prime the needle referred to as an ‘air shot’ by dialling up 2 units and pointing the needle towards the sky and pushing insulin through the needle. Make sure you can see a small amount of insulin at the top of the needle before dialling up your dose. This makes sure you get the correct dose and gets rid of any air bubbles that may be in the insulin pen/vial or cartridge. The air itself is not dangerous but it can lead to your insulin dose being less than what you expect.
- You do not need to pinch up the skin unless advised otherwise by your doctor, diabetes nurse practitioner or diabetes educator. Hold the skin firmly and insert the needle at 90 degrees (a right angle).
- After injecting the insulin, leave the needle in place under the skin for 10 seconds as this reduces the risk of insulin leaking out of the injection site and ensures you get the full dose of insulin.
- Dispose of used needles into a hard plastic container such as yellow sharps bin available from your local council or participating pharmacy.
These 3 steps can lower your risk of lipohypertrophy, injection site pain and bleeding, and potential infections:
- using a new needle for each injection
- select an appropriate injection site
- regularly rotate injection sites
Sticking to these steps will help your insulin to be absorbed in the same way with each injection, which will in turn help keep your glucose levels in target.
For more information, read the NDSS Insulin Fact Sheet
You can call our Diabetes Victoria Clinic on 1300 437 386 to book an appointment or visit the website for more information.









